Eye trauma is cause of ocular morbidity
that can be prevented1. It is one of the
leading causes of blindness2-4. Every year about 1.6 million people
become blind due to ocular trauma5. Eye injury results in a large
number of hospital visits6. Ocular trauma results in significant physical,
psychological and economical loses7. Eye injury results in
functional disability, cosmetic blemish, economical loss and psychological
distress. Impact of eye injury is long lasting and disturbing for the patient
and the whole family. Impact of ocular injury and vision loss is greatest in
magnitude compared to the loss of any other sensory organ of the body. Eye
injuries can occur in a variety of settings like during playing, in home, at
work or as a result of assault or accident8. Due to their anatomical
location and consistency eyes are prone to get hurt event by trivial trauma. Ocular
trauma can be profession specific as persons engaged in certain professions are
likely to get hurt by certain objects9. Every year around 55 million
people get injuries in their eyes. One out of every twenty patients coming for
eye examination by an ophthalmologist is a sufferer of eye injury10.
Trauma to eye can lead to immediate damage or it can lead to establishment of
inflammation and infection afterwards. Sequel of ocular trauma can cause
significant ocular morbidity even after months or years11. Self
medication by the patients or improper management by the quacks is another
contributing factor in morbidity related to ocular trauma. Ocular trauma is
often preventable and proper management of ocular injuries can significantly
lessen the burden of blindness12.
Data about ocular trauma
is limited in developing countries in terms of aetiology, setting, extent of
injury, pattern of injury and management strategies. As depending on occupation
and socio-demographic factors, nature and characteristics of ocular injury
differ from region to region, so we want to know the frequency and
characteristics of ocular trauma in Lodhran. Good knowledge of aetiology of
trauma, patterns and characteristics of trauma and at-risk population is needed
to device strategies for prevention and management of this disabling condition.
Proper resource allocation for the prevention and treatment of ocular injuries
can be planned according to burden of ocular injuries in the region.
MATERIAL AND METHODS
This cross-sectional study was conducted at
Shahida Islam Teaching Hospital affiliated with Shahida Islam Medical College,
Lodhran from December 2016 to September 2018. Sample size was calculated
according to the following formula:
S=Z2 p(1-p)/M2
S is sample size
Z is Z score its value is
1.96
P is population proportion
assumed to be 50% or 0.5
M is margin of error that
is taken 5% or 0.05
S = (1.96)2 (0.5)(1-0.5)/0.05
= 384.16
= 384
All ocular trauma patients presenting in the
out patients department and emergency department who required hospital
admission were included in the study. All patients were told about the purpose
of the study and informed consent was taken.
Demographic profile like age and gender of
all patients were recorded. History regarding aetiology of injury, eye
structures involved, place where injury occurred and pattern of injury were
recorded.
Ocular injuries were graded according to
Birmingham eye trauma terminology into two types namely closed globe and open
globe injuries. Closed globe injuries were further divided into contusion and
lamellar laceration. Open globe injuries were divided into laceration and
rupture. Mechanism of rupture was trauma with blunt object while trauma with
sharp object resulted in laceration. Laceration was further divided into
penetrating, perforating and presence of intraocular foreign body13.
Periorbital and adnexa injuries were recorded.
Record was taken of the time elapsed
between injury and presentation to hospital. Presenting visual acuity was
recorded with Snellen’s chart. Detailed ocular examination was performed with
the help of slit lamp biomicroscopy. B-scan and X-ray imaging were performed
when required.
All the information was
gathered with the help of specially designed proforma. Statistical analysis was
performed with SPSS version 23. Mean and
standard deviation was calculated for age. Frequencies and percentages were
calculated for gender, aetiology of injury, type of injury, structures
involved, place of injury, presence of hyphema, status of lens, presence of
vitreous haemorrhage, status of retina, optic nerve status, presenting visual
acuity, time lapse between injury and presentation to hospital and prolapse of
intraocular contents.
RESULTS
There were 393 patients
included in this study. There were 272 (69.2%) males
and 121 (30.8%) females. Mean age of patents was 28.97
± 12.59 years. Distribution of cases according to gender and age is shown in
table 1. There were 198 (50.4%) closed globe
injuries and 195 (49.6%) open globe injuries. The most common cause of injury was trauma with metal
object. The distribution of cases according to trauma is given in table 2.There were 132 (33.6%) cases of contusion, 99 (25.2%)
cases of rupture, 66 (16.8%) cases of lamellar laceration, 59 (15.0%) cases of
penetration, 27 (6.9%) cases of intraocular foreign bodies and 10 (2.5%) cases
of globe perforation. Cornea was involved in 146 (37.2%) cases,
corneoscleral injury was present in 126 (32.1%) cases, sclera in 46 (11.7%) cases
and adnexa in 27 (6.9%) cases. There was lid tear in 12 (3.1%) cases,
periocular swelling in 16 (4.1%) cases and blow out fracture was noted in 2 (0.5%)
cases. In 18 (4.6%) cases posterior segment was the predominant site of injury.
Hyphema was present in 186 (47.3%) cases, lens damage was present in 128 (32.6%)
cases, vitreous
Table 1: Distribution of cases according to gender and age.
|
Age of Patient in years |
|||
|
Gender of Patient |
Mean (Years) |
Number
of Cases |
Std.
Deviation |
|
Male |
28.20 |
272 |
14.108 |
|
Female |
30.70 |
121 |
8.030 |
|
Total |
28.97 |
393 |
12.597 |
Table 2: Distribution of cases according to
aetiology.
|
Injury Aetiology |
Frequency |
Percent |
|
Metal |
53 |
13.5 |
|
Wood/Vegetable matter |
49 |
12.5 |
|
Stone |
26 |
6.6 |
|
Road Traffic Accident |
35 |
8.9 |
|
Wielding arc |
10 |
2.5 |
|
Acid (chemical) |
18 |
4.6 |
|
Alkali (chemical) |
18 |
4.6 |
|
Superglue (chemical) |
16 |
4.1 |
|
Oil |
15 |
3.8 |
|
Fist/hand |
19 |
4.8 |
|
Fall |
11 |
2.8 |
|
Fire work/Fire cracker |
18 |
4.6 |
|
Fire |
9 |
2.3 |
|
Pellet gun |
27 |
6.9 |
|
Plant sap |
7 |
1.8 |
|
Insect fall/bite |
14 |
3.6 |
|
Animal attack |
11 |
2.8 |
|
Glass |
21 |
5.3 |
|
Plastic Scale/Pencil/Pen |
12 |
3.1 |
|
Tennis Ball |
4 |
1.0 |
|
Total |
393 |
100.0 |
Table 3: Distribution of
cases according to place of injury.
|
Place of Occurrence |
Frequency |
Percent |
|
Work place |
81 |
20.6 |
|
Road traffic accident |
44 |
11.2 |
|
Home |
95 |
24.2 |
|
Sports |
31 |
7.9 |
|
Assault |
58 |
14.8 |
|
At school |
24 |
6.1 |
|
Outdoor |
60 |
15.3 |
|
Total |
393 |
100.0 |
Table 4: Distribution of cases according to time to
presentation in Hospital.
|
Time to Presentation |
Frequency |
Percent |
|
Within 1 day |
131 |
86.2 |
|
Within 1 week |
17 |
11.2 |
|
After 1 week |
4 |
2.6 |
|
Total |
152 |
100.0 |
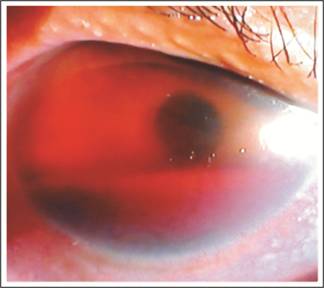
Fig. 1:
Hyphema as a result of blunt ocular trauma.
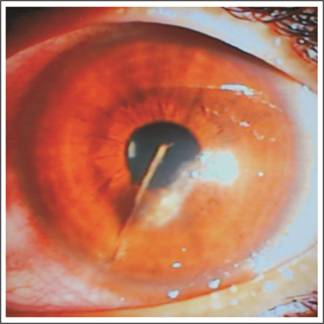
Fig. 2:
Ocular penetration with vegetable matter.
haemorrhage was present
in 103 (26.2%) Cases, retinal tear was present in 13 (3.3%) cases, retinal
detachment was present in 29 (7.4%) cases, commotio retina was present in 22
(5.6%) cases. Optic nerve swelling was noted in 32 (8.1%) cases. Distribution
of cases according to place of injury is given in table 3. Presenting visual
acuity was 6/12 or better in 139 (35.4%) cases, between 6/12 and 6/60 in 98
(24.9%) cases and less than 6/60 in 156 (39.7%). Distribution of cases according to time to presentation
in hospital is shown in table 4. Prolapse of intraocular contents was noted in
122 (31.0%) cases.
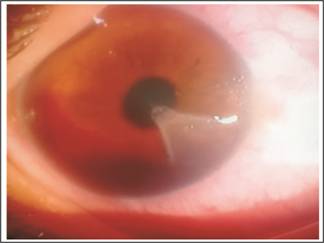
Fig. 3:
Lamellar corneal laceration with hyphema.

Fig. 4: Limbal perforation, Iris and vitreous
prolapsed following ocular trauma with Key.
DISCUSSION
Ocular trauma is one of the major causes of
preventable blindness and visual impairment14.
Three hundred and ninety-three patients with ocular trauma were included in
this study. Mean age of patients was 28.97 ± 12.59 years. Results of our study
are similar with the findings of study done by Dhulikhel that showed the most
vulnerable age group was 21-30 years15. Study
of Godar and co-authors also recognized the most vulnerable age group for
ocular trauma was between 21 to 29 years. Ocular trauma in young age group may
be due to their increased risk-taking behaviour and active life style.
Morbidity resulted thereof has great impact in terms of economical burden and
quality of life.
There were 272 (69.2%) males and 121
(30.8%) females included in our study. Work performed by Sengupta and
co-authors also showed the preponderance of male patients affected by ocular
trauma16. Increase ocular trauma in male
patients may be due to their increase outdoor activity and engagement in
certain professions17.
In our study there were 198 (50.4%) closed
globe injuries and 195 (49.6%) open globe injuries. Among closed globe injuries,
contusion was the most common cause. Among open globe injuries, globe rupture
was the most common cause. Our results are similar to findings of other
studies. In our study most common cause of injury was metal object and cornea
was involved in majority of cases. Our results are in accordance with the
result of other studies18.
In our study most common place of injury
was home. Our results are in contrast with the results of other studies19 where most of ocular trauma occurred at
work place and during road traffic accidents. Our results are in accord with
that of the study conducted by Shaeri and co-authors20. Due to
inadequate adoption of safety measures during common house hold activities may
be reason for majority of ocular trauma at home. Most of the trauma among women
and children occur at home. It is irony that home environment that is
considered the safest accounted for majority of ocular trauma. Adoption of
safety measures at home while doing house hold activities is as much needed as
during outdoor activities.
In our study time to presentation to
hospital was within one day in 342 (87.0%) cases, within 7 day in 41 (10.4%)
cases and after 1 week in 10 (2.5%) cases. Our results are comparable to that
of Godar and coauthors14.
In our study presenting visual acuity was less
than 6/60 in 156 (39.7%) while in another study conducted by Sengupta and co-authors
majority of patients presented with visual acuity less than 3/6016. This
is in contrast with the result of study conducted by Iqbal and co-authors19.
In their study majority of patients presented with good visual acuity. This
difference in presenting visual acuity may be due to severity of ocular trauma.
In our study we included patients who required hospital admission. Patients
with minor ocular trauma were not included in our study.
Among the limitations of our study is the small
sample size. This study may not be true representative of population as patients
from high socioeconomic strata were unlikely to come to public hospital.
Patients who needed hospital admission were included in our study. This is
another limitation. Patients with minor injuries who did not need hospital
admission or did not come to hospital were not included in the study.
Nevertheless, our study
underscores the frequency and patterns of ocular trauma in particular locality.
It will help establish preventive and management strategies to cope with ocular
trauma. Future research is needed to study the impact of health education on
adaption of safety measures in preventing ocular trauma. Moreover, it will be
important to study the anatomical and physiological outcomes of ocular trauma
management strategies.
CONCLUSION
Ocular trauma occurred
more commonly in males. Ocular trauma was blunt and occurred in home setting in
most of the times. The aetiological agent in most of the eye injuries was metal
and wood. Ocular injuries resulted in substantial visual loss at the time of
presentation.
Author’s Affiliation
Dr. Muhammad Luqman Ali
Bahoo
Associate Professor and
Head of Ophthalmology, Shahida Islam Medical College, Lodhran.
Dr. Ahmad Zeeshan Jamil
Associate Professor of
Ophthalmology, Sahiwal Medical College, Sahiwal.
Dr. Beenish Karamat
Resident Medical
officer, Department of Radiology, LGH.
Author’s Contribution
Dr. Muhammad Luqman Ali
Bahoo
Concept, Study Design,
interpretation of data
Dr. Ahmad Zeeshan Jamil
Drafting of article and
critical revision for important intellectual content
Dr. Beenish Karamat
Statistical analysis,
literature research and proof reading
Conflict
of interest: None.
Financial
disclosure: None.
REFERENCES
1.
Bahoo MLA, Jamil AZ.
Types of ocular surface foreign bodies and their correlation with location in
the eye. Pak J Ophthalmol. 2018; 34 (1): 25-9.
2.
Jan S, Khan S, Khan MT, et al. Ocular emergencies. JCPSP. 2004; 14: 333-6.
3.
Guerra Garcia RA, Garcia D, Martinez FE et al. The Cuban ocular trauma registry. J Clin Exp Ophthalmol. 2013; 4
(2): 276.
4.
Negral AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998; 5:
143-69.
5.
Tsedeke A, Yeshigeta G, Fessehaye A. A 2 year review of ocular trauma in Jimma University specialized
hospital. Ethiop J Health Sci. 2009; 19: 67-74.
6.
Babar TF, Khan MN, Jan S, et al. Frequency and causes of bilateral ocular trauma. JCPSP. 2007; 17:
679-82.
7.
Bahoo MLA, Jamil AZ, Khalid MS. Ocular surface foreign bodies and their association with
profession. PJMHS. 2018; 12 (2): 495-8.
8.
Khatry SK, Lewis AE, Schein OD, et al. The epidemiology of ocular trauma in rural Nepal. Br J
Ophthalmol. 2004; 88: 456-60.
9.
Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal. Br J
Ophthalmol. 2004; 88: 456-60.
10. Magarakis
M, Mundinger GS, Kelamis JA, Dorafshar AH, Bojovic B, Rodriguez ED. Ocular injury, visual impairment and blindness associated with
facial fractures: a systematic literature review. Plastic and reconstructive
surgery, 2012; 129: 227-33.
11. Bowling,
B. Kanski's clinical
ophthalmology a systematic approach, 2015; Sydnery: Saunders.
12. Pandita
A, Merriman M. Ocular trauma
epidemiology: 10-year retrospective study. N Z Med J. 2012; 125: 61-9.
13. Kuhn
F, Morris R, Witherspoon D, et al.
A standardized lassification of ocular trauma. Ophthalmology, 1996; 103: 204-3.
14. Godar
ST, Kaini KR, Amatya P, Joshi K, Singh L. Magnitude of ocular trauma in a tertiary care hospital of western
Nepal. NJMS. 2013; 2 (2): 140-3.
15. Sthapit
PR, Marasini S, Khoju U, Thapa G, Nepal BP. Ocular Traumain patients presenting to Dhulikhel Hospital.
KathmanduUniv Med J 2011; 33: 54-7.
16. Sengupta
P, Mazumdar M, Gyatsho J.
Epidemiology of ocular trauma cases presenting to a tertiary care hospital in a
rural area in West Bengal, India over a period of 2 years. IOSR-JDMS. 2016; 15:
92-7.
17. Hussain M, Moin M, Aasi NA. Epidemiology of
Penetrating Trauma. Annals of KEMC
(Lahore) 2003;9(2):163-166.
18. Oum
BS, Lee JS, Han YS.
Clinical features of OcularTrauma in Emergency Department. Korean J Ophthalmol.
2004; 18: 70-8.
19. Iqbal
Y, Khan QA, Zia S, Malik A.
Frequency and characteristics of ocular trauma in Gilgit, Pakistan. JIIMC.
2016; 11: 157-62.
20. Shaeri
M, Moravveji A, Fazel MR, Jeddi FR. Status of ocular trauma in hospitalized patients in Kashan, 2011:
As a sample of industrial city. Chin J Traumatol. 2016 Dec. 1; 19 (6): 326-329.